For the first time in years, Amina Lawal's children slept through a rainy season without falling ill. The 32-year-old mother of three in northern Nigeria is grateful for the dual-ingredient mosquito net she received last year, part of a new set of malaria-prevention tools being distributed across her region.
"Every rainy season would bring with it fear of mosquito-borne diseases," Amina tells TRT Afrika. "The new net and the vaccine my children received at the clinic now feel like a real shield. We are sleeping in peace."
Healthcare agencies are spreading this new safety net, which combines a standard pyrethroid insecticide with a second active ingredient like chlorfenapyr or pyriproxyfen, across malaria-endemic parts of Africa.
The World Health Organisation (WHO) notes in its annual World Malaria Report that newer tools like these dual-ingredient nets and recommended malaria vaccines helped prevent an estimated 170 million cases and a million deaths in 2024 alone.
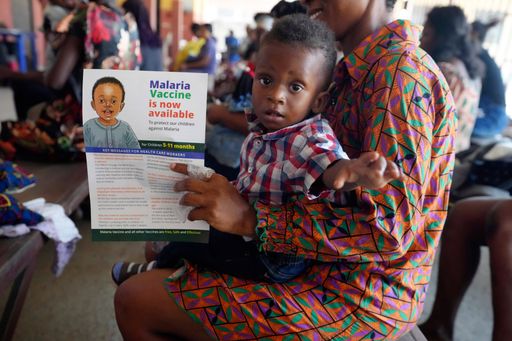
Since 2021, as many as 24 countries have introduced malaria vaccines into their child immunisation programmes.
Seasonal malaria chemoprevention, another strategy where children in endemic zones like the Sahel receive monthly doses of anti-malarial drugs, has helped protect 54 million children annually across 20 countries. Back in 2012, the number of children who benefited from this was barely 200,000.
A few countries have already eliminated malaria while some are within achievable distance of the goal. WHO certified Cabo Verde and Egypt as malaria-free in 2024. Georgia, Suriname and Timor-Leste joined the list this year, taking the total to 47 countries and one territory.
Pockets of worry
Amid all the encouraging signs, parts of the continent are reporting what community health worker John Mwangi terms an "alarming shift" in malaria patterns.
"The medicines are not working like they used to," Mwangi, who works in the highlands of western Kenya, tells TRT Afrika.
"We have children coming in and getting the usual treatment, but the fever lingers. It also takes longer to recover now. It seems both the vector and the parasite are adapting. We are in a race where the finish line keeps moving."
Mwangi's observation reflects the central concern of this year's report. Despite the life-saving impact of new tools, an estimated 282 million malaria cases and 610,000 deaths were recorded in 2024, which works out to nine million more cases than the year before.
Africa accounted for 95% of those deaths, mostly children under five. Even more worrying, the foundation of malaria treatment is under threat.
WHO reports that anti-malarial drug resistance, centred on artemisinin derivatives, is now confirmed or suspected in at least eight African countries.
"New tools for prevention of malaria are giving us new hope, but we still face significant challenges," says WHO's director-general, Dr Tedros Adhanom Ghebreyesus.
He also warns that rising cases, drug resistance, and funding cuts threaten to roll back two decades of progress.
Besides drug resistance, rapid diagnostic tests are becoming less reliable due to parasite mutations. Insecticide resistance in mosquitoes is widespread too.
Anopheles stephensi, a resilient mosquito species, is now the primary cause of malaria in nine countries of the continent.
Extreme weather events and conflict are additional risk factors, one fuelling outbreaks and the other crippling health systems.
Funding shortfall
Globally, US $3.9 billion went into malaria prevention in 2024, but it was still less than half the $9.3-billion target.
"The World Malaria Report shows that drug resistance is increasing. Our response must be equally strong," says Dr Martin Fitchet of the open-source research organisation Medicines for Malaria Venture.
He points to the development of the first non-artemisinin combination therapy as the start of a "new chapter in malaria resilience".
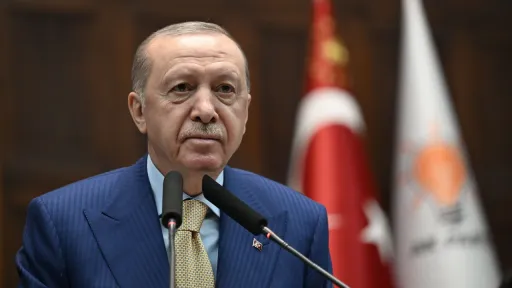
The path forward, as outlined in the WHO report, demands a strengthened "country-led, partner-enabled" response that hinges on translating political commitments like those in the recent Yaoundé Declaration into action and resources.
The fight is focused on scaling up the distribution of life-saving tools that are working while simultaneously innovating to outpace drug and insecticide resistance.
For Amina in Nigeria, the new tools mean a quiet night. For John in Kenya, they represent a fading hope unless reinforcements arrive. The million lives saved last year prove a malaria-free future is possible.
"We finally have a shield," Amina tells TRT Afrika. "We pray it does not break."